Kirsten H.
On March 8th 2019, I woke up feeling completely normal. At 9am I caught the bus to work and felt a sharp intense pain in my right side. By the time I got to work I was in overwhelming pain, and headed to the hospital. A CT scan revealed a 3mm kidney stone in my right kidney. I was relieved as I thought this was the least dangerous scenario. I was sent home with opiates, Tylenol, and antibiotics and told I would feel better in 1-3 days.
At 3am I woke up shivering uncontrollably, with my whole body shaking and my teeth chattering. I remember feeling like I might die and talking myself down, because that seemed so illogical. I had a fever of 104.7 degrees so I got up, had a Tylenol, a popsicle and a cold shower. My fever went down and I went back to sleep.
When I woke up at 7am, I went to grab my phone to tell my boss that I was too sick to work. I was unable to lift my arm. Holding my phone felt like holding a 50lb weight and I could barely move my fingers to text. I was not in any pain and I had no fever. I called the nurses hotline and they told me to call an ambulance.
As soon as I got to the hospital, they put me straight into emergency. The first nurse came up to take my blood pressure. As the air filled on my arm band I saw a shocked and concerned look wash over his face. He tapped my wrist and looked like he had just seen a ghost. He said, "You should be dead right now." Within minutes a group of doctors, nurses and a respiratory specialist all appeared. They put in my IV and catheter and then the respiratory doctor started explaining to me what drugs he would be putting me on. As he walked away to grab the medicine I started to feel short of breath. My partner went to grab a nurse and I coughed. When I looked down into my hands they were filled with several cups of bright red blood. This was when I realized something was terribly wrong.
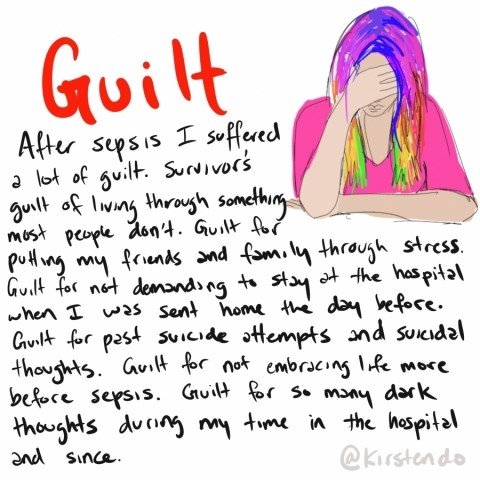
Instantly the emergency room turned into chaos. It seemed like dozens of people were racing around and yelling. A nurse held my hand and said "This is the best ICU in Canada, do not worry you are not going to die." Up until this point I hadn't considered death an option. A second later I dozed off from the drugs.
I woke up the next day on life support. I had a feeding tube in my nose and a breathing tube down my throat. I had 13 tubes total in my body, including a nephrostomy tube draining urine from my right kidney. I found out that I had septic shock and multiple organ failure caused by urosepsis. The 3mm stone was stuck in ureter, causing a blockage that resulted in an infection. The infection spread to my internal organs including my lungs, heart and brain within a matter of hours. Because I was on opiates from the day before I did not feel most of the symptoms. I was told I would be in the ICU for around 3 weeks and the hospital for around 3 months.
The ICU was the worst place I have ever been. I was the only patient not in a coma, and all the other families were going through so much emotional distress. My lungs kept filling with blood and the nurses would have to use suction device all the way down my breathing tube. The second day in the ICU they said I was improving quickly and by the third morning I was good enough to leave the ICU. They took out my breathing and feeding tube and I was sent to the general medicine ward.
At this point my lungs were still full of blood and I could not walk on my own, sit up, or use my arms very much. I was grateful to have my breathing tube out as I was able to talk and I was feeling alert. Over the next 7 days I progressed quickly. On day 5 I was able to go to the bathroom with my walker and graduated from diapers to pull-ups. On day 7 I was able to shower and go outside. By day 8 I got my catheter out, I could walk up and down stairs, and wear normal underwear. On day 9 I was sent home with just a nephrostomy tube and a home-care team to help change the dressing on my tube every 2-3 days.
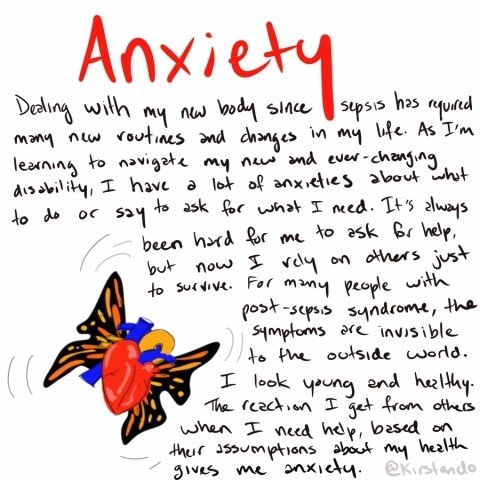
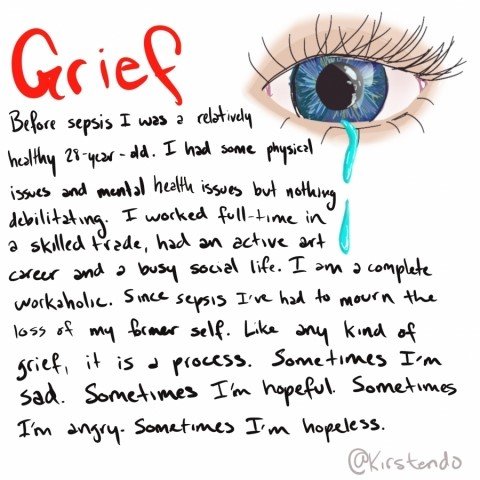
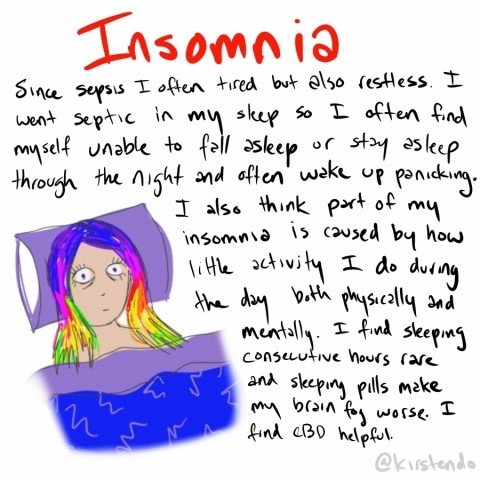
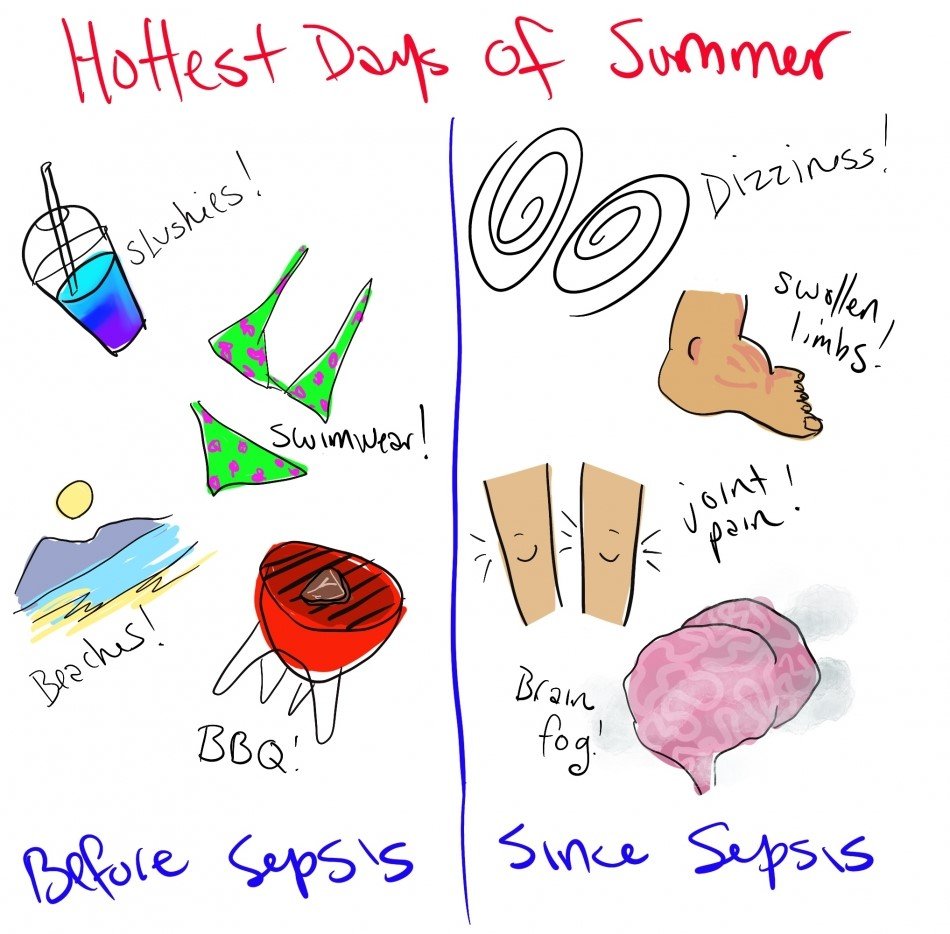
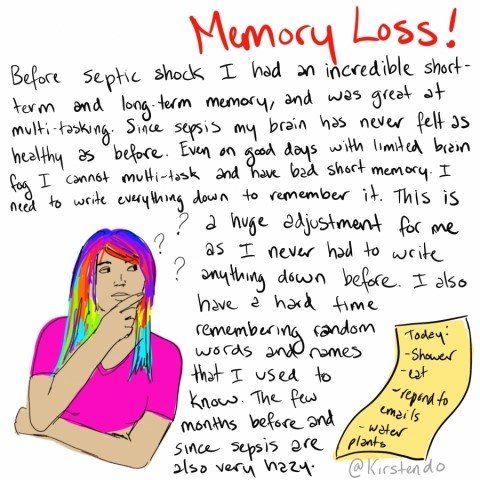
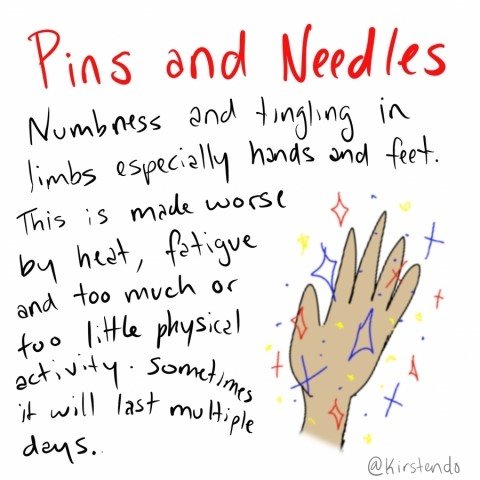
I thought my recovery would continue to go quickly because I got better so quickly in the hospital. At first it did, but as time progressed my symptoms started to plateau. I am now 6 months post sepsis and not even close to feeling back to "normal". I am unable to work and even being social is exhausting. My symptoms were constantly fluctuating and on a good day I was always questioning myself on how bad my bad days actually were.
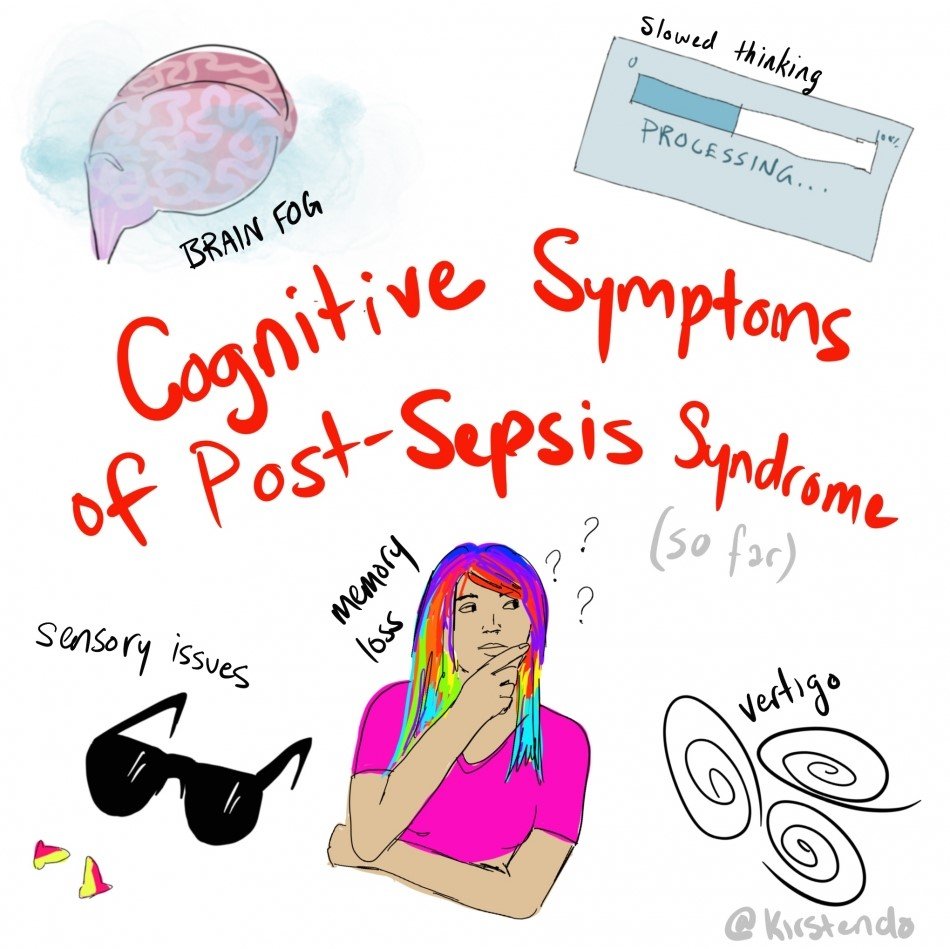
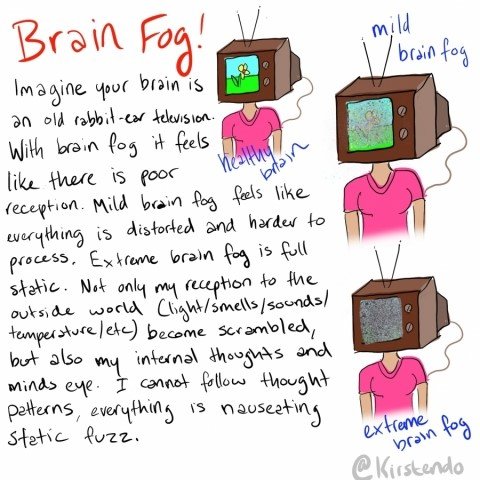
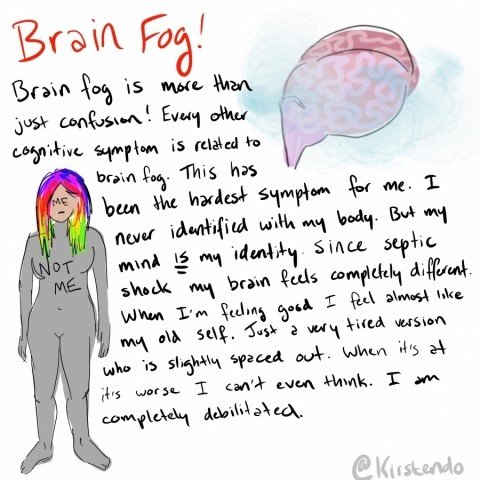
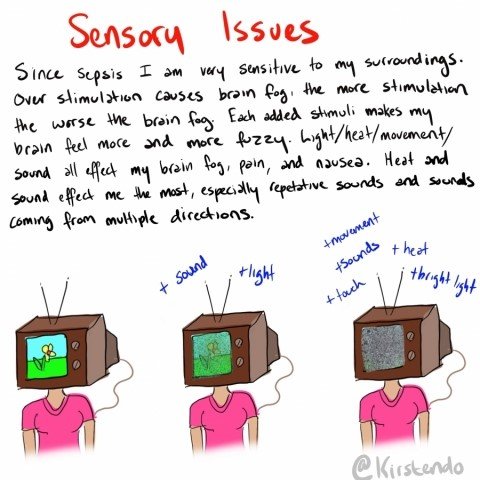
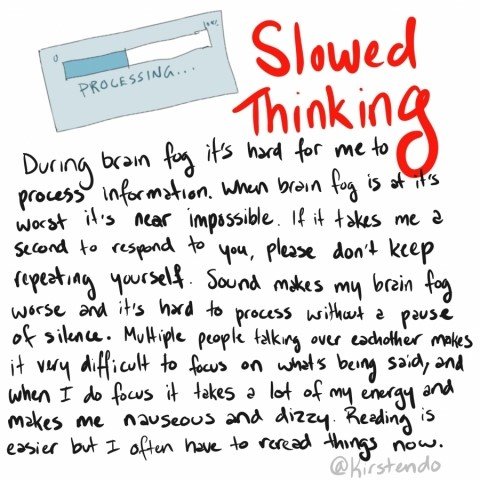
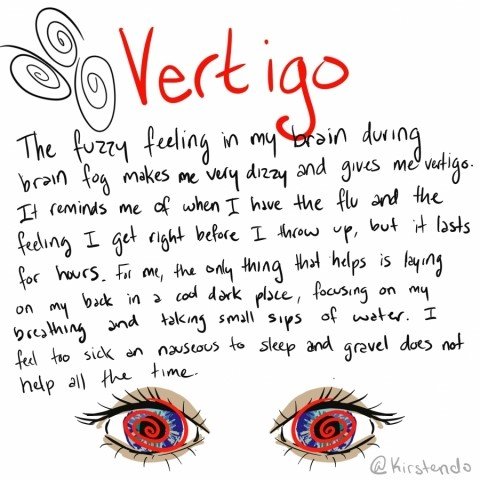
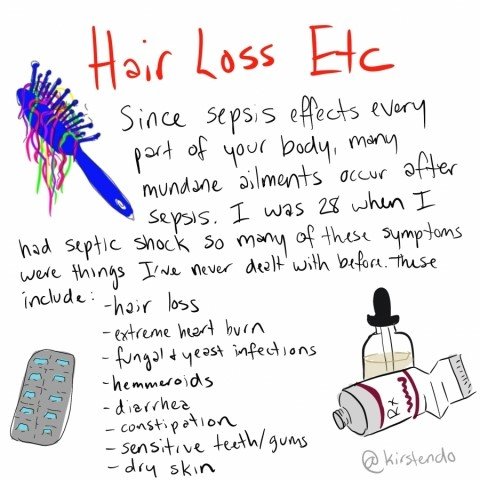
Eventually I joined a post-sepsis support groups and realized we all share the same symptoms - symptoms that were very specific, but that I never found information on from any good searches into post-sepsis syndrome. I decided to start making comics as an educational tool, for myself and for others going through the same thing. It’s hard when you look healthy but are so sick. People do not believe you. I had so much frustration asserting my illness to friends and family and having them brush it off. Those who have not seen my comics still brush it off but I found them to be an incredible tool for help others understand post-sepsis syndrome.
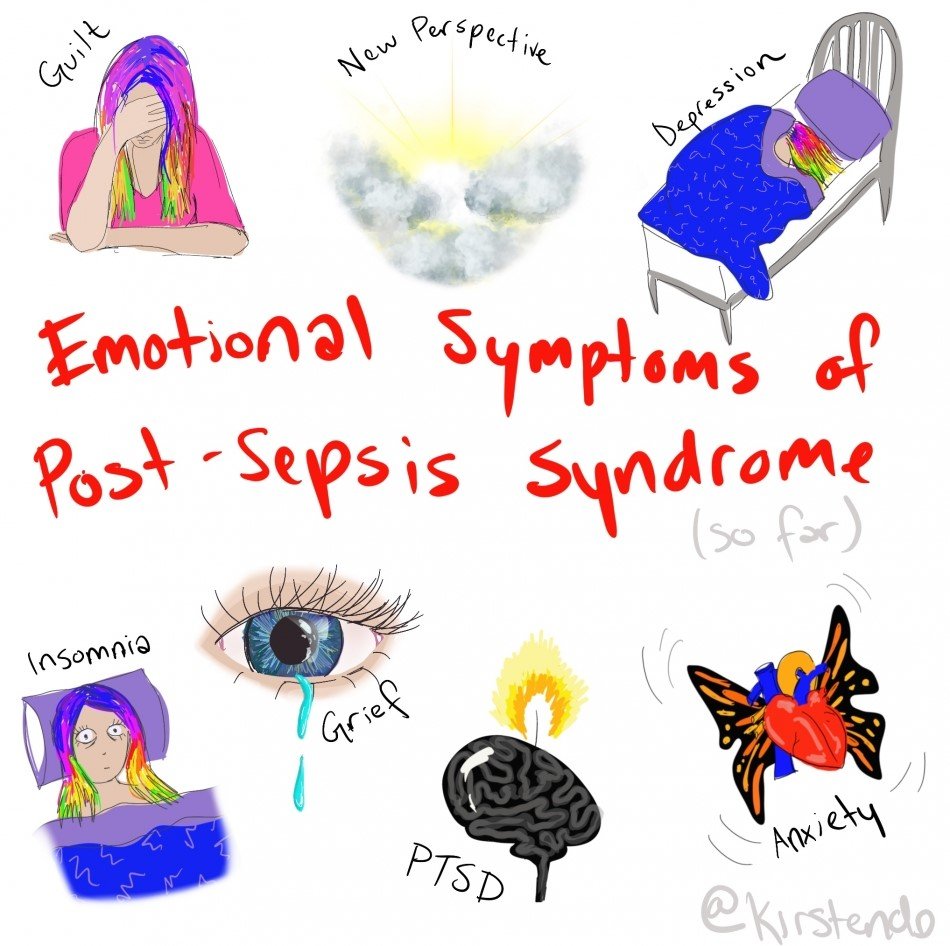
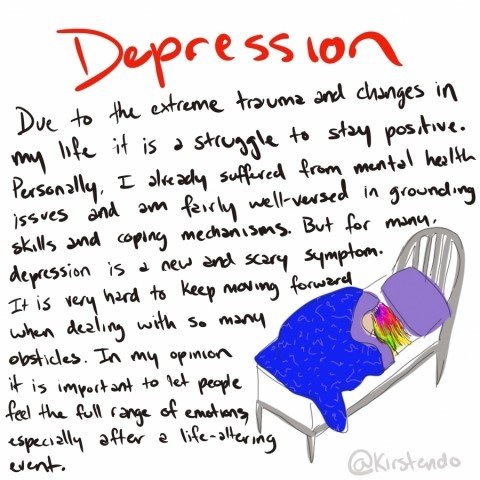
Learn about the emotional, cognitive, and physical symptoms of Post-Sepsis Syndrome, told through Kirsten’s comics below.